Pancreas Transplant
A pancreas transplant is an operation to replace a diseased pancreas with a healthy one from someone who’s died. It’s a complex procedure with risks of complications, and it requires lifelong immunosuppressant drugs. But pancreatic transplantation is the only treatment close to a cure for severe, uncontrolled long-term Type I diabetes.
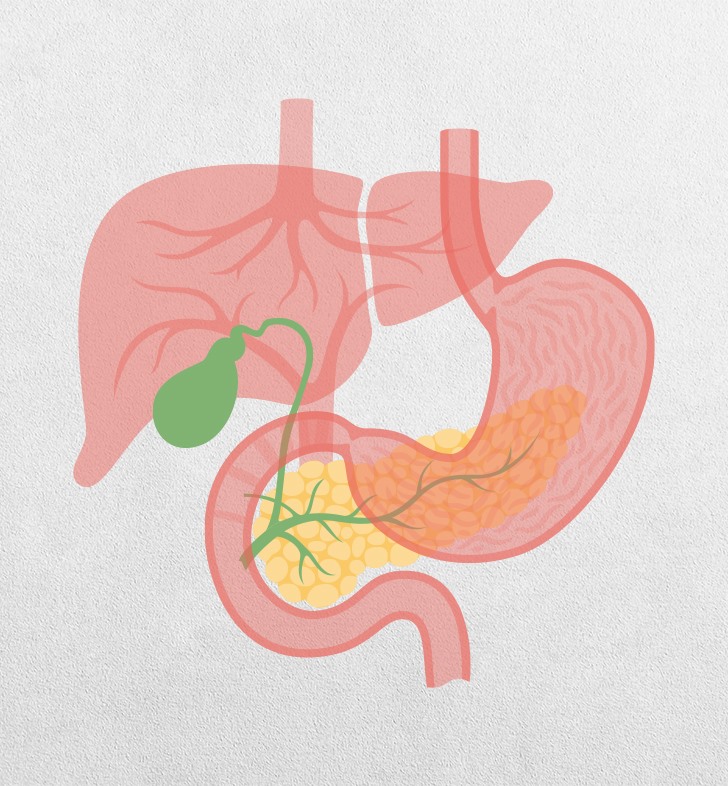
What is a pancreas transplant? A pancreas transplant is an operation to replace a diseased pancreas with a healthy one from a deceased donor. Who needs to have a pancreas transplant? Pancreas transplantation treats severe, long-term, uncontrolled Type 1 diabetes, also called insulin-dependent diabetes. Your pancreas is an organ behind your stomach. It produces insulin, a hormone that helps your body use sugar (glucose) for energy. In Type 1 diabetes, the pancreas makes little to no insulin. People with Type 1 diabetes must inject insulin to help control blood glucose levels. Sometimes insulin injections are not enough to control diabetes. Eventually, a lack of insulin and uncontrolled high glucose levels can cause damage throughout your body. Kidney disease is one of the most severe complications of Type 1 diabetes. Most people who are eligible for a pancreas transplant also have kidney failure. A pancreas transplant is often performed at the same time as a kidney transplant. With a healthy pancreas from a transplant, a person with diabetes can begin to produce insulin (insulin independence).
Why is a pancreatic transplant done? Pancreas transplantation is the only treatment that’s close to a cure for Type 1 diabetes. The surgery can help you live a longer, fuller life. A transplant can end the need for: Daily monitoring of blood glucose. Insulin injections. Food restrictions. Risk of diabetes complications.
What happens before pancreas
transplantation?
If your healthcare provider thinks
you might be a candidate for a pancreas transplant, you will need:
Blood work and urine tests to make
sure you’re healthy enough for surgery.
History and physical exam.
Immunological study, which helps the
transplant team match you with a compatible donor.
Imaging tests (for example,
ultrasound, MRI) to make sure you’re healthy enough and to help plan surgery.
Psychological evaluation to make
sure you understand the surgery and its risks.
If the transplant team believes
you’re a candidate, they’ll place you on a national waiting list for a
pancreas. Many people are on the waiting list for months or even years before a
matching pancreas is available.
What should I do while I wait for a
pancreas transplant?
Your healthcare team will coach you
on ways to stay healthy while you wait for surgery, such as:
Attending all of your medical
appointments.
Avoiding smoking.
Exercising regularly if you’re
healthy enough.
Limiting alcohol.
Reporting any changes in your health
to the transplant team.
Taking medications exactly as
prescribed.
Surgery should happen as soon as
possible after a matching pancreas becomes available. Other ways you can
prepare for surgery include:
Making sure the transplant team can
contact you at all times.
Packing a bag for the hospital so
you’re ready to go on short notice.
Telling friends, family and your
employer about your situation so they can plan to act quickly to support you.
What happens during pancreas
transplantation?
A pancreas transplant takes about
three to five hours (almost twice as long for a combined kidney and pancreas
transplant).
You’ll be asleep under general
anesthesia the entire time, so you won’t feel anything. The surgeon will:
Make incisions (cuts) along your
belly from below your breastbone to below your belly button. Sometimes the
surgeon makes additional incisions in your groin, between your abdomen and
thigh.
Place the donated pancreas along the
right side of your abdomen.
Attach it to nearby blood vessels
and your small intestine (part of your digestive system).
Leave your original pancreas in
place so it can still produce digestive juices.
Close the incisions with stitches.