Aortitis
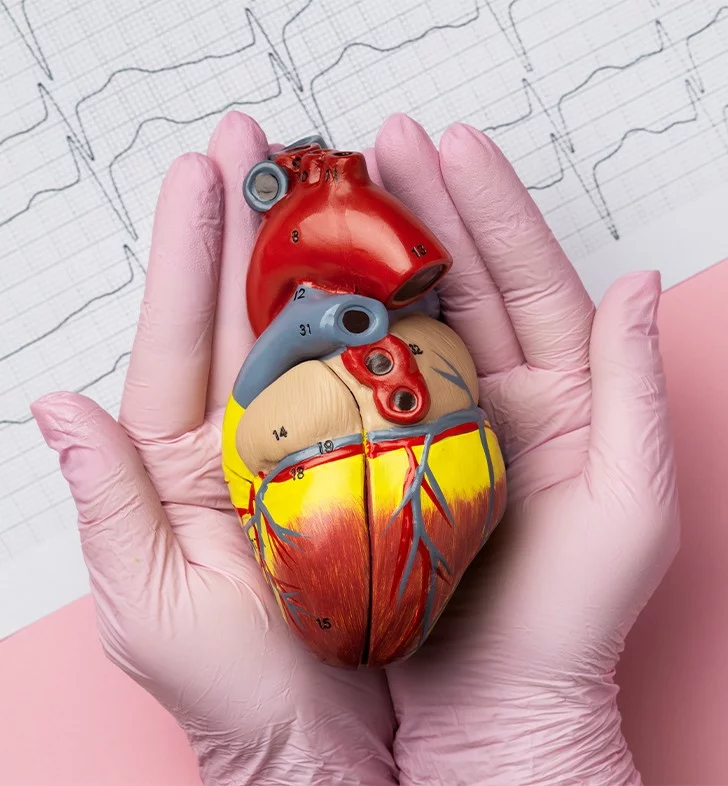
What is aortitis? Aortitis refers to inflammation of your aorta. The aorta is the largest artery you have in your body and it has branches that provide blood flow to all of your body’s organs and tissues. As the aorta is a blood vessel, aortitis is one potential manifestation of vasculitis, or blood vessel inflammation. Aortitis can occur in isolation or together with inflammation of other blood vessels (systemic vasculitis). There are many different types of systemic vasculitis. Healthcare providers identify these by the blood vessels the condition affects and other features. Aortitis can widen your aorta, creating an aortic aneurysm, or possibly make your aorta narrow (aortic stenosis). These can be life-threatening because your aorta is your body’s biggest handler of oxygen-rich blood that goes to your body. Several factors influence your symptoms, diagnosis and treatment: What part of your aorta the condition affects. If there’s inflammation of other blood vessels. If your provider identifies an underlying cause or associated disease.
Is aortitis an autoimmune disease? Yes, in most instances healthcare providers consider vasculitis (blood vessel inflammation) to be an autoimmune disorder. This means your body is causing inflammation of its own tissues.
How common is aortitis? The underlying disease or cause that the aortitis is occurring in association with affects how frequently aortitis occurs. In general, aortitis is uncommon.
What are the symptoms?
Aortitis symptoms may be different from person to person, depending on if they occur in the setting of an underlying vasculitis or an associated inflammatory or infectious disease.
In some instances, people with aortitis may not have any symptoms.
Aortitis symptoms may include:
Chest pain.
Stomach (abdominal) pain.
Back pain.
Headache.
Vision changes.
Fever.
Shortness of breath.
Swelling in your legs.
Pain in your arms or legs with use.
Symptoms of inflammation such as decreased energy, weight loss or loss of appetite.
Symptoms related to vasculitis affecting other blood vessels.
Symptoms related to an underlying disease if this is present.
How else can aortitis affect my body?
In addition to the symptoms they have, people with aortitis can have complications, including:
Kidney failure.
Stroke.
Heart attack.
Heart failure.
Rupture or tearing of the aorta.
What causes aortitis?
Aortitis can occur as part of an underlying systemic vasculitis or related to another inflammatory disease. In these settings, the actual cause of the underlying disease and the associated aortitis is unknown. Also, certain infections can cause aortitis.
Providers may find aortitis unexpectedly at the time of aortic surgery. When aortitis isn’t associated with another underlying disease or cause and it’s not affecting other blood vessels, this is called “isolated focal aortitis.”
Systemic vasculitis and other inflammatory disorders
Giant cell arteritis.
Takayasu arteritis.
Cogan syndrome.
Behçet disease.
Kawasaki disease (almost exclusively affects children).
Polyarteritis nodosa.
Other forms of systemic vasculitis.
Ankylosing spondylitis.
Rheumatoid arthritis.
Systemic lupus erythematosus.
Relapsing polychondritis.
Sarcoidosis.
Immunoglobulin 4 (IgG4)-related disease.
Inflammatory bowel diseases.
Infections
Salmonella.
Syphilis.
Staphylococcus.
Rocky Mountain spotted fever.
Gonococcal infection.
Tuberculosis.
Hepatitis B and C.
Herpes viruses.
Fungal infections.
How is aortitis diagnosed?
To make an aortitis diagnosis, your healthcare provider will:
Talk to you about your medical history.
Do a physical exam.
Order imaging tests to look at your aorta and all of its major branches.
Order blood tests that can show a high level of inflammation in your body.
Evaluate your aortic tissue under a microscope if you’ve had surgery on your aorta.
What tests will be done to diagnose aortitis?
Imaging tests for aortitis may include:
Echocardiogram.
Transesophageal echocardiogram.
Abdominal ultrasound.
Computed tomography (CT).
Magnetic resonance imaging (MRI).
Positron emission tomography (PET).
Blood tests may include:
Erythrocyte sedimentation rate.
C-reactive protein.
Complete blood counts.
Chemistries to check kidney and liver function.
Other blood tests to look for systemic vasculitis, other inflammatory diseases or infection if necessary.
Aortic tissue examination:
If you’re having surgery for an aortic aneurysm, your surgeon may take a tissue sample during surgery to check for inflammation. Some people with no prior symptoms or signs of aortitis get an aortitis diagnosis at the time of their aortic aneurysm surgery.
How is aortitis treated?
The treatment of aortitis can include medication and/or surgery. Providers base their treatment decisions on:
Which part of your aorta the condition affects.
If the aortitis is causing an aneurysm or a narrowing and how severe this is.
Whether there’s an associated disease or other underlying cause.
If it’s affecting other blood vessels.
You may not need treatment if you have isolated focal aortitis that a provider found and completely removed during aortic surgery and there’s no underlying disease. In such settings, ongoing monitoring remains extremely important to ensure there are no new features that develop that may warrant a different approach.
What medications are used for aortitis?
Your healthcare provider will use medications when they identify an underlying active systemic vasculitis, other inflammatory diseases or an infection. They may recommend:
Anti-inflammatory or immunosuppressive medicines for systemic vasculitis or other underlying inflammatory conditions.
Antibiotic drugs for aortitis associated with an infection.
Are there side effects of these treatments?
Immunosuppressive medications reduce your body’s ability to fight an infection. Your healthcare provider will discuss the risks and benefits of each treatment as well as strategies to reduce these risks.
When do I need surgery for aortitis?
You may need surgery if you have:
An aortic aneurysm that’s sufficiently large where there’s a concern for rupture or where the aneurysm is affecting heart function.
A narrowing in your aorta that’s seriously reducing blood supply to other vital body sites.